(Butler, PA) On-site therapists or on-site therapy rooms could benefit the mental health of nurses overwhelmed by COVID-19 caseloads and staff shortages, according to Butler County Community College registered nursing students who may enter the high-priority occupation in 2022.
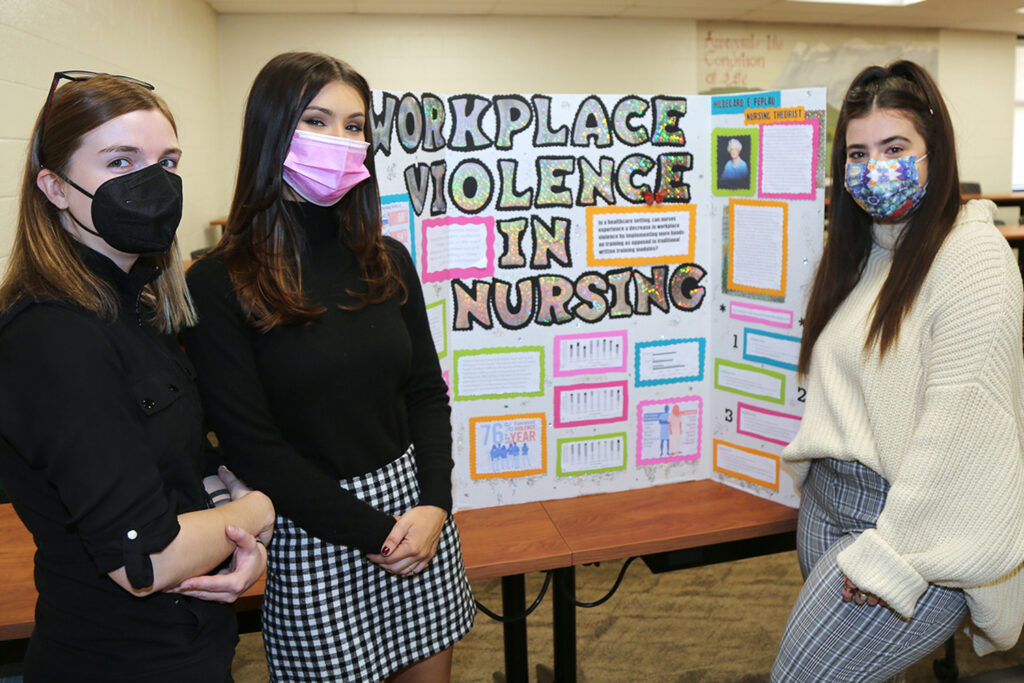
Second-level students – those who expect to graduate in May from the Nursing, R.N., career program held on BC3’s main campus – from seven Pennsylvania counties researched in groups issues confronting health care and presented proposals recently in the college’s business and health professions building.
Issues included “workplace violence in nursing,” “ventilator-associated pneumonia with mouth care as the intervention,” “communication boards vs. no communication boards in relation to patient care and safety” – and “on-site therapy to reduce burnout in the critical care nurse.”
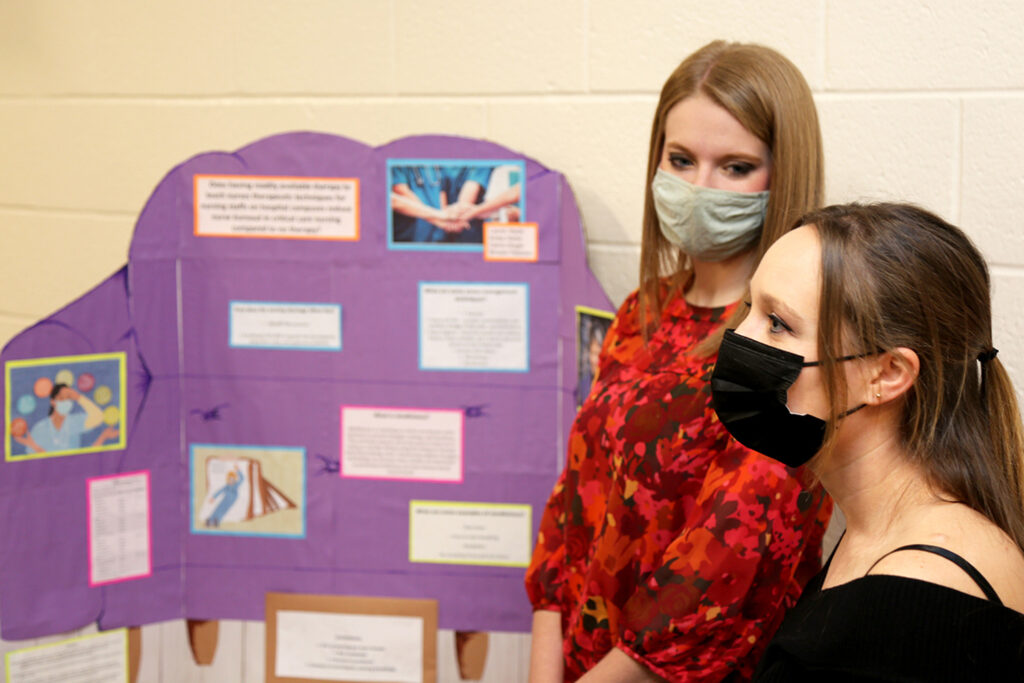
Carrie Dingel, Krista Hartle, Brooke Peterson and Lauren Wade are among BC3 main campus Nursing, R.N., students who attend clinical experiences at regional health care facilities, where nurses can be affected by the succession of COVID-19 patients and by increased hours to compensate for colleagues who have left the field.
“Burnout is crazy high,” said Hartle, of Butler. “There’s already a shortage on staff. You’re picking up extra shifts. You’re trying to take care of critically ill patients. You’re running on zero energy.”
“Burnout is crazy high. There’s already a shortage on staff. You’re picking up extra shifts. You’re trying to take care of critically ill patients. You’re running on zero energy.”
Krista Hartle, BC3 Nursing, R.N., student
“It’s something they are seeing in the present,” said Dr. Patty Annear, dean of BC3’s Shaffer School of Nursing and Allied Health. “It’s a problem.”
“Not only do we have sicker patients, we have more patients coming in,” said Heather Darrington, a BC3 faculty member who also works as a critical care nurse at a regional hospital. “We have more nurses leaving the bedside because of the burnout. And that creates even more burnout.”
If nurses do not take care of themselves, Annear said, “They are not going to be able to care for others.”
“It’s really hard to see their patients die”
More than 11,540 COVID-19 cases were reported Dec. 9 in Pennsylvania, the most in any single day since Dec. 10, 2020, according to the state Department of Health.
Roughly 85 percent of the 3,600 intensive-care unit beds in Pennsylvania were occupied as of Dec. 13, according to the Johns Hopkins University of Medicine’s Coronavirus Resource Center, which compiles statistics from the U.S. Department of Health and Human Services. Nearly half of the intensive-care unit beds occupied were by patients with COVID-19.
Additionally, Darrington said, “Pre-COVID, more of the critical care patients were being transferred to the floors rather than heading out to their own funerals. … It’s taxing on a nurse’s mental health.”
Dingel, Hartle, Peterson and Wade point to research that indicated that 75 percent of nearly 200 nurses who responded to a Journal of Clinical Nursing survey during the pandemic reported moderate, severe or extremely severe stress.
Sixty-five percent reported moderate, severe or extremely severe depression.
And nearly 60 percent, moderate, severe or extremely severe anxiety.
“I think it’s really hard to see their patients die, or to know they are going to pass away,” said Peterson, of Renfrew. “That is a really hard thing to deal with every day.”
A place to “decompress”
Their proposal for health care facilities is on-site therapists or on-site therapy rooms.
“As the pandemic continues, a lot of people are focusing on mental health,” said Wade, of Butler. “Taking care of the people who are eventually going to be taking care of others should be a high priority.”
“A spot to go to where they can decompress,” said Dingel, of Cabot. “You would see a lot of improvement.”

That spot could include a massage chair, students said. Or a space for yoga or other stress-management techniques. Painted possibly in therapeutic colors, and quiet.
And having access to a therapist in-person or remotely, where critical care nurses could discuss stress, Wade said, “and how to deal with it.”
“Having someone to talk to and feel safe,” Wade said. “You can talk to your co-workers all the time, but if you are at the nurses’ station and you are afraid your supervisor is going to hear you, you’re not going to be completely honest about how you feel.”
A number of health care systems have employee assistance programs for workers to access therapy, Darrington said, “but not quite on-site.
“On-site is important because it would be somewhere a nurse could go while on shift, or it’s close by. You don’t have to leave work or drive somewhere else. When you are working a 16-hour shift, that does not give you a lot of time to make a therapy appointment somewhere where the therapist may be open only 9 to 5.”
“It’s going to take a toll”
Their idea may be beneficial to any health care worker, Peterson said, including social workers and home care nurses.
Watching patients die “on a regular basis, no one can … no matter how resilient you are,” Peterson said. “It’s going to take a toll on your mental health.”
Registered nursing is a 2021 high-priority occupation in the Tri-County and West Central workforce development areas, which include Armstrong, Butler, Lawrence and Mercer counties.
More than 275,000 registered nursing positions will be available through 2030, according to the U.S. Department of Labor’s Bureau of Labor Statistics.
About 1,000 registered nurses in Armstrong, Butler, Lawrence and Mercer counties are 55 or older, according to EMSI, a labor market research firm based in Idaho.
More than 75 percent of BC3’s Class of 2021 in registered nursing received one or more job offers or had interviews scheduled before completing the college’s two-year career program in May.
Second-level BC3 Nursing, R.N., students
BC3 students expecting to graduate from BC3’s 70-credit main campus Nursing, R.N., program in May researched issues confronting health care and presented proposals Nov. 23.
Those from Armstrong County are Mackenzie Dean, Dayton; Christina Denardo and Colleen McGarrity, Ford City; Bailey Anthony and Jonathan Brake, Kittanning; Abigail Branan, Manorville; and Ruth Ann Bradford, Worthington.
Those from Butler County are Butler residents Brianna Collins, Brooke Dingel, Jared Fechter, Kaley Fitzpatrick, Holly Goettler, Krista Hartle, Julia Kleinfelder, Casey Kretzer, Bailey Lewis, Frances Martin, Nicole Miller, Beth Rhodaberger, Bethany Rhodaberger, Emma Scuotegauzza, Heather Snow, Clairise Snyder, Lindsey Stover, Sarah Vasas, Lauren Wade, Julia Williamson, Megan Wilson and Jaela Yohe.
Those from Butler County are also Carrie Dingel, Cabot; Rhiannon Morin, Cranberry Township; Evans City residents Michaela Buxton and Michelle Gaiser; Joy Davis, Harrisville; Mars residents Nicole Hillman, Chelsea Walker and Shyniah Watson; and Abigail Kingerski, Portersville.
Those from Butler County are also Renfrew residents Taylor Gilliland and Brooke Peterson; Kylie Godlewski, Sarver; Saxonburg residents Brittney Barnett, Kelsea McConnell and Veda Reiser; and Maryna Boychenko, Seven Fields.
Those from Butler County are also Slippery Rock residents Shannon Glenn and Alexandra Gray; Lauren Wiles, West Sunbury; and Marcie Delaney, Zelienople.
Those from Mercer County are Grove City residents Skylar Bowers, Chelsie Kerns and Megan Meyerl; Natasha Myers, Jamestown; and Lily Keller, Sandy Lake.
Others are Beaver County residents Allison Chronister, Fombell; and Jessica Hoover, Freedom; Lawrence County residents Jennifer Cassandro, Ellwood City; and Miranda Sadler, New Castle; Kassandra Smith, Shelocta, Indiana County; and Crystal Bowser, Vandergift, Westmoreland County.





